Integrating Quality Improvement in HIV Programs (Pre Exposure Prophylaxis)
Introduction
HIV incidence is high in Blantyre, especially among the key population (MSM, FSW, and partners of FSW) and AGYW. New interventions are being implemented without effectively integrating the learning component for quality improvement. The intervention is addressing issues around suboptimal coordination and low uptake of PrEP in Blantyre city. PrEP is effective scientifically but there is a need to address quality issues for proper implementation and obtaining maximum gains from the intervention. Having a higher incidence among the key population and the city thinks if PrEP is effectively implemented then Blantyre city can be able to reduce HIV incidence. The higher the incidence of HIV among the vulnerable populations the greater the risk of city residents getting HIV. That also translates into an increase in the HIV prevalence rate. This means that the HIV burden in the city will not reduce.
The intervention has the following objectives;
• Develop data-driven, community-informed, responsive, and adaptive prevention programs that are attractive to at-risk populations
• Deliver quality HIV prevention services through coordinated public and private delivery channels at the community and facility level to populations most at risk of HIV acquisition
• Measure program performance, quality, and effectiveness of prevention programs in reducing incidence to adapt and expand user-provider interfaces as needed.
Description
Through the PrEP QI Collaborative, we strengthen QI structures at both district and facility levels. This is done to enable the city/district and facilities to be capable of using QI methods to improve the quality and uptake of HIV prevention services including PrEP and expand the targeting of these services to the at-risk population The main activities within the program are;
- QI capacity building for facility-based QI team, district QI mentors team, and leadership through monthly QI mentorship
- Testing of change ideas along the PrEP cascade to improve access and quality of services
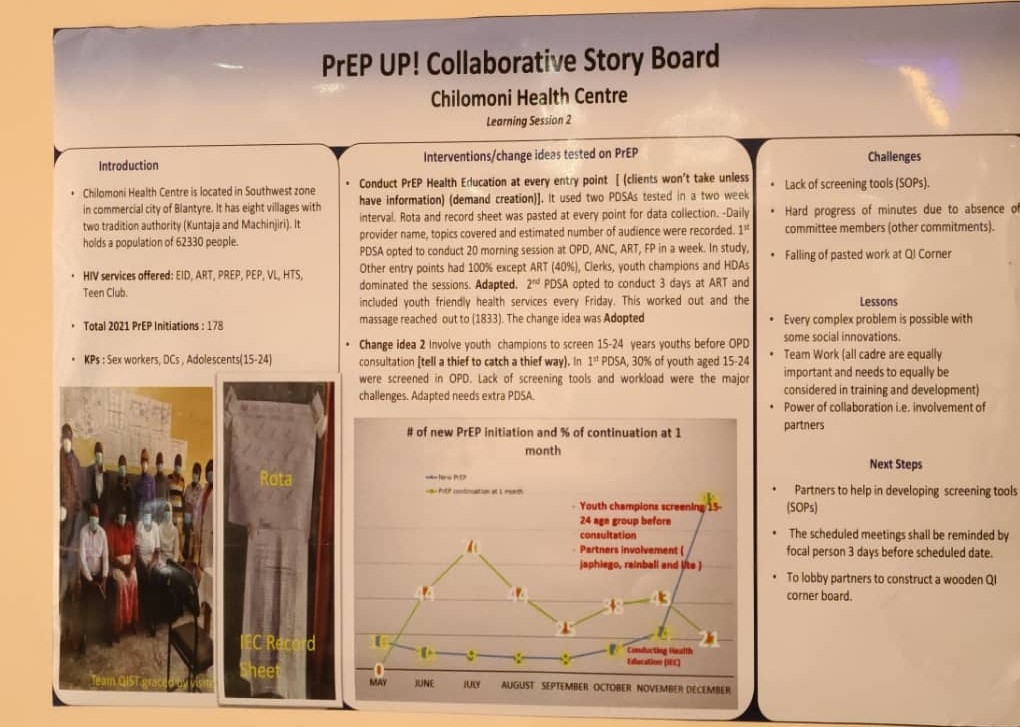
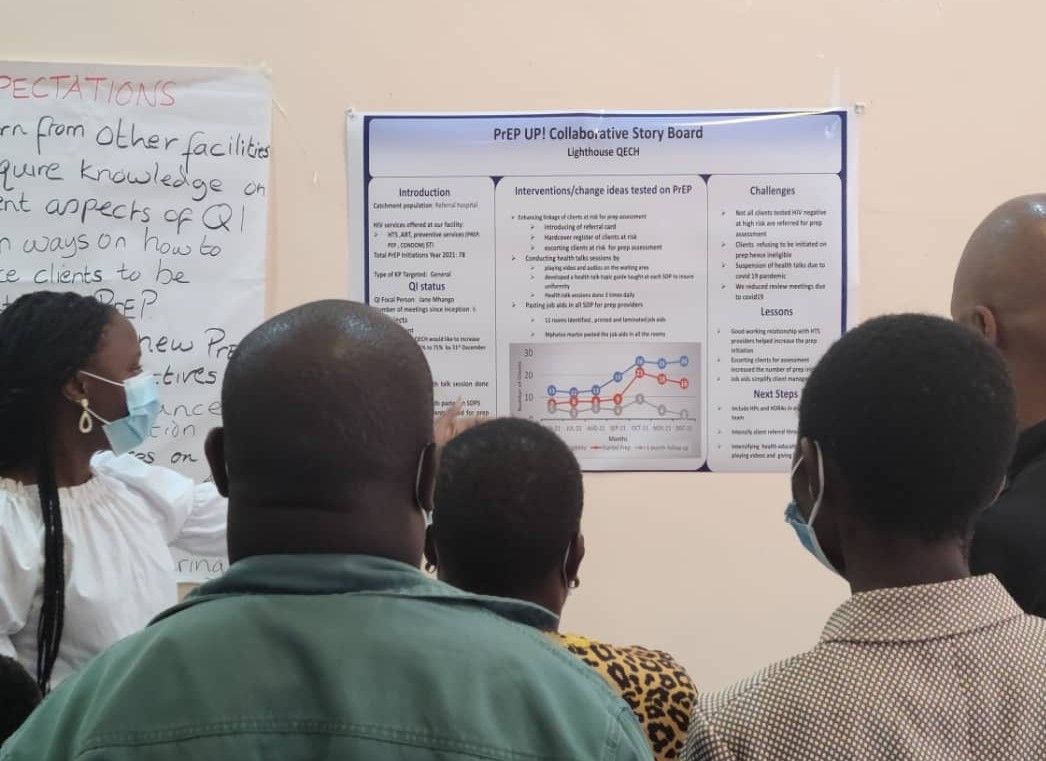
- Providing a platform for sharing best interventions through collaborative learning sessions. Meetings are conducted quarterly with representatives from all health facilities providing PrEP and PrEP partners.
- Data deep dives on PrEP data and other HIV-related data to inform facility and district actions. Each facility makes a poster presentation highlighting its achievements, challenges, and plans for the following quarter.
- Sharing of demand creation for PrEP through health education and distribution of IEC materials The activities are implemented in 21 health facilities in Blantyre which make up the PrEP UP! Collaborative.
The QIC was launched in September 2021 with the first learning session however pre-work activities started in August 2020. PrEP collaborators include DHO, DREAMS project, EGPAF, MACRO, IAPAC, Lighthouse, PAKACHERE, Queen Elizabeth Central Hospital, University of Malawi, and Cooper Smith among others Below are some of the indicators monitored for the program • Process data to inform the quality of the PrEP delivery process and QI program processes o No. of people screened for PrEP eligibility o No. of people eligible for PrEP o No. of people enrolled for PrEP o No. of people retained on PrEP at 1 and 3 months • Outcome data focusing on outcome indicators for the PrEP program • QIC has 9 indicators ( both process and Outcome) • Data is collected every month by facility data officers and sent to HIMS under the ministry of health
Data Collection
Data is collected every month by facility data officers and sent to HIMS
Results, Outputs, and Outcomes
- QI structure which includes district QI leadership, a team of district QI mentors, and facility-based QI teams are up and functional.
- QI leadership which includes district QI focal person and HIV prevention coordinators strengthened and led QI collaboration in Blantyre
- 20 QI mentors trained and mentored now leading QI coaching and mentoring in Blantyre
- 88 facility based QI team members trained in QI methods
- 22 QI teams strengthened through QI coaching and mentoring now leading to the testing of changes ideas to accelerate the uptake of PrEP in Blantyre
- 44 data officers oriented on data management for improvement.
- As of December 2021, 21 facilities had integrated PrEP into their services from 7 facilities at baseline (March 2021)
The table below shows program outputs on a quarterly basis for 2021.
|
Quarter |
No. of people assessed |
No. of people initiated |
% increase in initiation/quarter |
% refused PrEP |
|
1 |
63 |
19 |
|
45.8 |
|
2 |
244 |
185 |
974 |
10.5 |
|
3 |
422 |
359 |
194 |
9.5 |
|
4 |
1080 |
836 |
233 |
12.4 |
The table above shows that after the project was introduced, only 19 people were initiated on PrEP out of the 63 screened during the first quarter. In the same quarter, about 45.8% of those screened refused to be initiated on PrEP. Due to collaborative learning, the project outputs changed from one quarter to the other, in quarter 2, the refusal rate significantly reduced and the number of people initiated on PrEP increased by 974%. In quarter 4 we had the highest number of PrEP initiations (1080) double the previous quarter. Currently, the project is working on increasing the retention rates. The project started with a 1 monthly retention rate of 43% and by end of December 2021 retention rate was now at 53%. For the 3 months retention, at the beginning of the program, this was at 38% and by end of December 2021, it had improved to 44%. The project is still working towards improving the retention rate.
So far the project has been successful in increasing the number of people assessed for PrEP, increasing the number of people initiated in PrEP, and increasing PrEP acceptance rate.
Lessons Learned
• Quality improvement methods, including process mapping, root cause analysis, and testing of changes, inform how to adapt systems to effectively deliver PrEP and other HIV prevention services routinely in health care facilities
• Integrating PrEP screening and demand creation in multiple service areas has shown promise in increasing PrEP uptake
• PrEP taskforces and designated champions facilitate agency-wide delivery and improvement of PrEP services
• Collaboration and coordination with key IPs are key to the success of PrEP implementation
• QI Mentor’s program approach is key to building QI capacity at district- and site-level
• Learning Sessions provide an important platform and forum for peer sharing and exchange of PrEP implementation successes and challenges
• The leadership of the DHO in another district is essential for replication. QI capability, including QI coaching, would need to be built if not present.
If relevant, Please describe the sustainability/continuity of the best practice within the context of the COVID-19 pandemic.
The leadership and mentoring team built at the district level through a QI focal person and a team of QI mentors respectively will provide oversight for the collaborative and continued QI coaching and mentoring to facility QI teams beyond the funding time frame. The QI teams at the facility and district level are well trained to implement the intervention. QI supervision visits can be integrated into other routine visits done by the district to facilities. Some of the activities can also be integrated into the District/city implementation plan for funding by the government. The Ministry of Health has a QI department with specialists who can ably implement the intervention.
Conclusion
The community has benefited from the high quality of PrEP interventions. The intervention has directed service providers towards the implementation of evidence-based PrEP interventions. The voice of the communities has been heard through this intervention. The intervention is considered a best practice because it is fully integrated into the District Health Office for implementation and support. The project has built the capacity of the facilities making them more sustainable. The concept of QI can also be integrated into other HIV interventions for implementers to learn and continuously improve their interventions.
Best Practice Type
- Intervention
City
- Blantyre
Best Practice Domain
Meeting the needs of key populations
Accelerating uptake of proven interventions/policies/diagnostics/medicines
Best Practice Primary Audience
Researcher/Academia
Health Department or Ministry of Health
Implementing Partner
Clinician